BY CYNTHIA MCGRATH | SEPTEMBER 14, 2021
To borrow from actor John Krasinski, we can all use some good news – especially in healthcare. One of our member school employees has a story that makes us smile. Are you familiar with a mobile hospital, also known as a mobile ER department and mobile urgent care? We weren’t, but we’re excited to share “Susan’s” experience.
Susan recently fell and suffered multiple fractures. She’s recovering well and has faithfully stuck to a strength and conditioning regimen to improve her mobility. While she was recuperating, she got an upper respiratory infection that required medical attention. Due to her lack of mobility, she couldn’t travel to the hospital without using an ambulance. Her doctor suggested using a mobile hospital service.

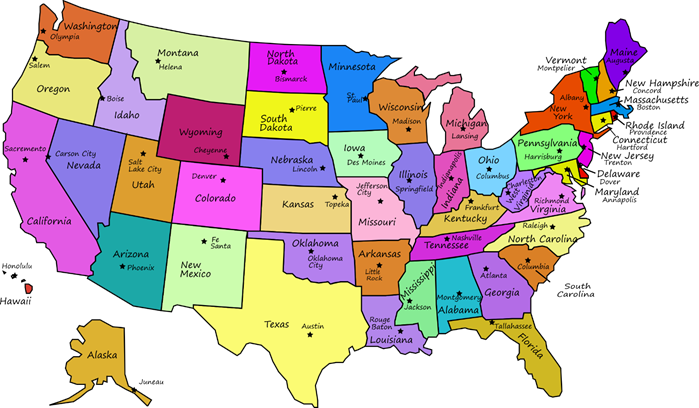
With the Delta variant of COVID raging across the country, staying out of an emergency room - unless it’s critical - is prudent. Emergency rooms are also very understaffed, leading to long waits for non-emergency issues. In response to overcrowding and significantly longer wait times in the emergency room, Rhode Island’s Department of Public Health recently urged residents to avoid the hospital for non-emergencies. Governors and hospital directors warn that the hospital staffing crisis is so acute that patients can no longer expect the level of care that might have been available six weeks ago, according to Politico.
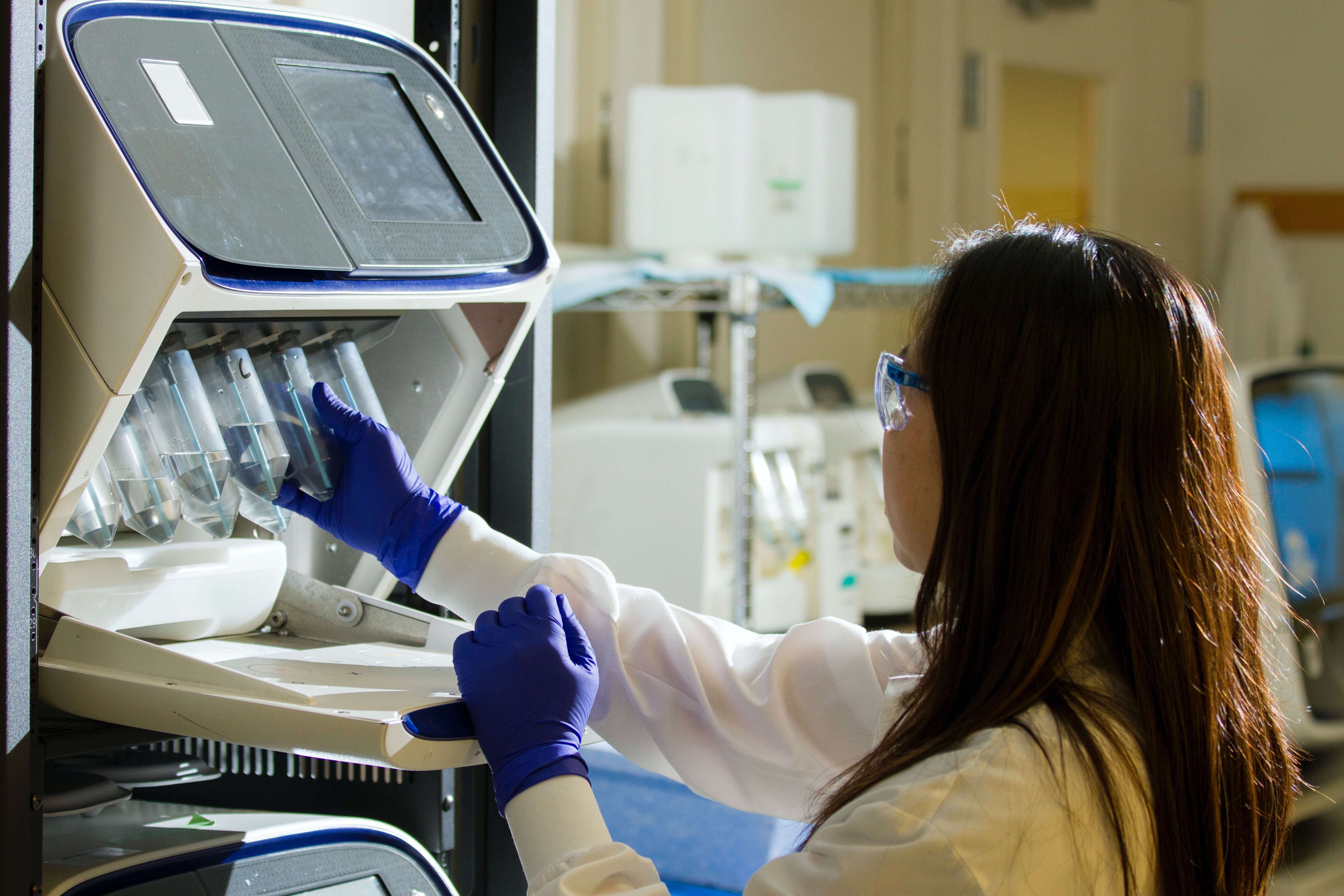
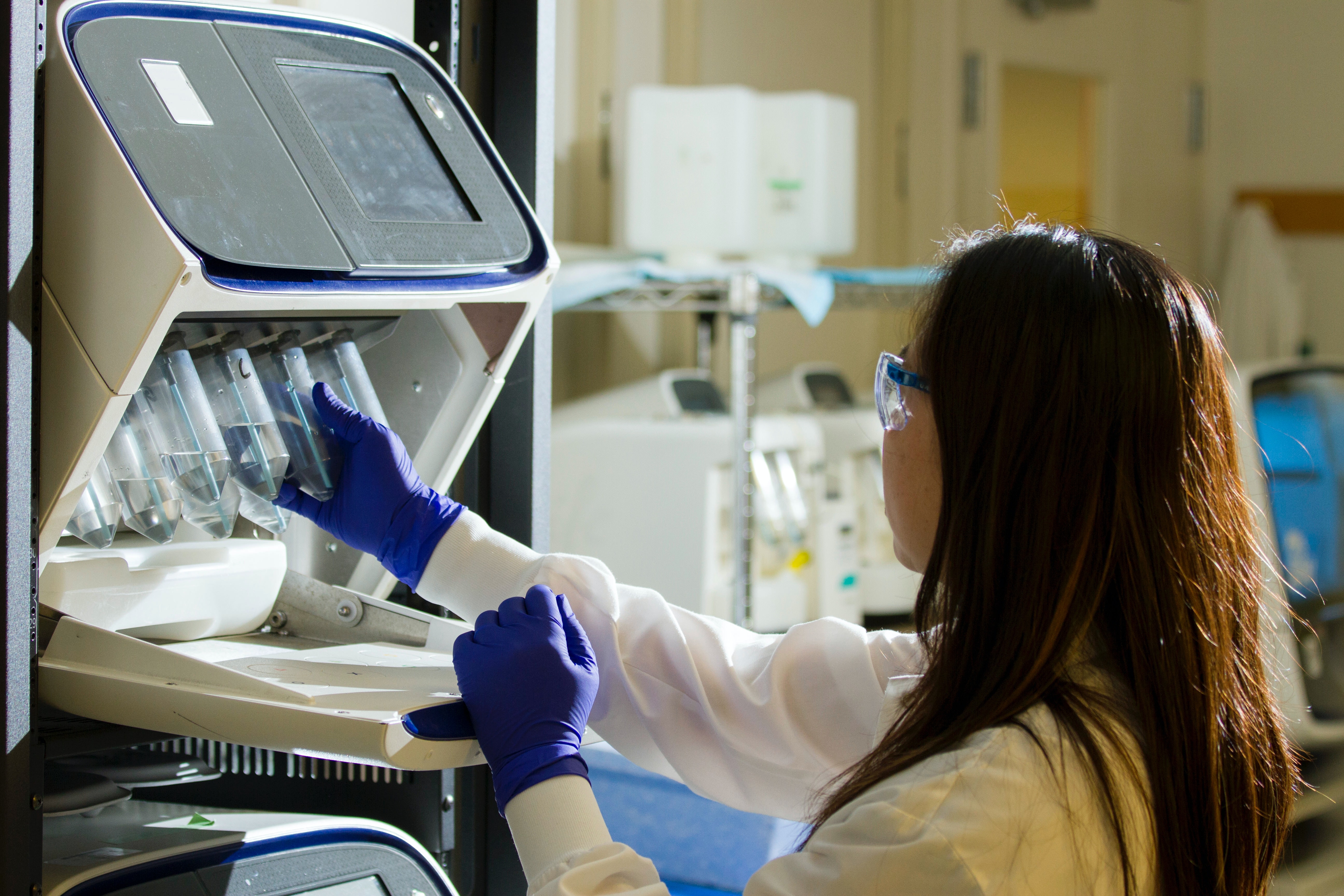
Our member school employee avoided all these worries and inconveniences. Two vans pulled up to her home soon after her doctor arranged for the service. They were staffed by an X-ray technician, a paramedic, and a trained phlebotomist. The team performed a chest X-ray in Susan’s kitchen, and the phlebotomist drew blood and a urine sample. They sent the results to an offsite doctor to read. “The technicians were the eyes, ears, and hands for the doctor,” said Susan. “The paramedic listened to my lungs and let the doctor, who was on video, know what she was hearing.”
Based on the results, Susan required an antibiotic. The van included a locked pharmacy to prevent theft. The team accessed a single pill via transmitted code and transmitted the full prescription to a local pharmacy. The doctor on video chat watched Susan ingest the pill. “This was a well-oiled machine,” said Susan. “I had a physical, chest X-ray, urinalysis, blood draw and doctor consult all within an hour, well short of what I would have spent at an emergency room.”
Susan also saved on out-of-pocket costs. She only paid $25 for the service compared with much higher emergency room charges. Significantly, she saved money on an ambulance ride. Although health plan benefits include ambulance services — with no cost or cost sharing, depending on the plan — many ambulance companies do not participate in provider networks. Fifty-one percent of emergency, and 39 percent of non-emergency, ground ambulance rides result in an out-of-network charge for privately insured Americans, according to the Peterson-Kaiser Family Foundation tracker.
Ambulances transport about 3 million people to emergency rooms each year. Approximately 10% of patients visiting the emergency room get there by ambulance. “I was in a non-ambulatory state due to my accident, and only needed the ambulance for transportation,” said Susan. “Avoiding that trip saved me a lot of money and I’d recommend this service to my mother.”
Susan’s good healthcare news – she received the highest caliber of healthcare quality that left her feeling confident and well-cared for while saving her money.