By CYNTHIA MCGRATH | February 4, 2019
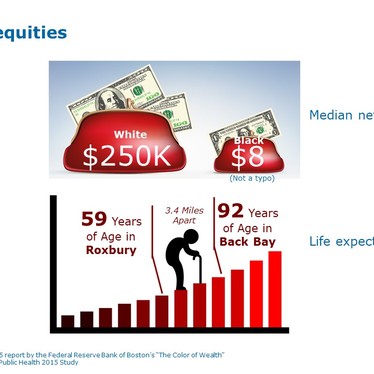
How do we go about improving care for our employees while reducing costs? That’s the conundrum facing most employer healthcare purchasers. According to Workpartners, edHEALTH’s data warehouse, 5% of our insureds represent over 50% of our claim costs. Our Board made the strategic decision to target these high-cost claimants. We believe it will be a triple win: an opportunity to reduce costs, improve care for our members, and benefit our participating schools.
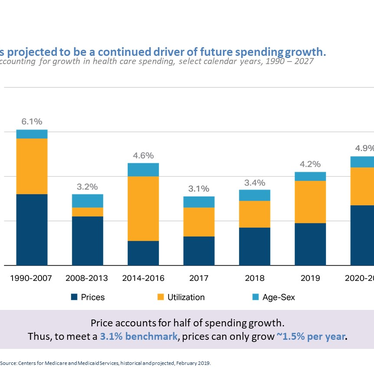
edHEALTH’s premium trends have consistently been lower than the industry. Over the last four years, we’ve averaged premium increases of 2.7% per year. That’s much better than national trends of 4.1% (Kaiser Family Foundation), and even better when employer cost shifting is factored in. We have made very few benefit changes since our inception in 2013.
The first step in launching our population health program was to identify our high-cost claimants. Our data warehouse uses a proprietary HUI (Human Capital Risk Score) score based on over 300 weighted risk variables to detect these individuals. On average, these patients visit 10 different providers, have 11 diagnoses and 32 tests, and have been prescribed 10 prescription drugs each year.
Those numbers demonstrate an opportunity for improved care coordination and communication. We’re offering our schools a clinical prevention program that provides personalized care for high-risk, high-cost employees and covered dependents. Through phone and secure email, participants receive support for medical decisions.
Have you ever left the doctor’s office and realized that you have questions? This happens all too often, but providers are busy, and it’s frequently difficult to connect with them. Our innovative clinical prevention program fills this gap. Participants can contact the clinical staff for answers about their diagnosis, treatments, tests, and medications. They also receive support for making lifestyle changes, reviewing their medications, and work/life balance.
The program’s information, education, and decision support helps decrease unnecessary costs and utilization. It complements - and doesn’t replace - programs offered through the health plans. Conversations and patient information are confidential and never shared with edHEALTH or the employee’s school.
Our participating schools benefit in many ways by participating in this program. There’s no cost the first year and they’ll receive periodic reports on edHEALTH’s population risk and the program’s Return on Investment. Early analyses show this program could measurably reduce claims spending for each participating school.
edHEALTH is proud of its work to keep healthcare premiums affordable, but we know we can’t be complacent. Effective population health programs like ours have the potential to improve care and reduce costs. And, that’s a winning strategy!
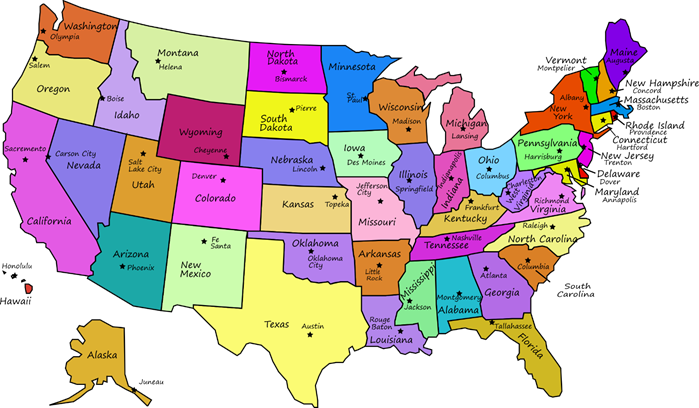
edHEALTH, established in 2013, is a collaboration of 25 higher education and secondary school institutions that own and govern the organization. By coming together to provide healthcare benefits, the members of edHEALTH realize lower costs than available through fully insured or go-it-alone self-insured options.